Awareness of female genital mutilation (FGM) in European countries has increased over recent decades as a result of globalisation and migration of populations. The World Health Organization (WHO) describes FGM as procedures that involve partial or total removal of the external female genitalia, or other injury to the female genital organs for non-medical reasons.
There is no medical indication for this practice, and it represents a human rights violation, an extreme form of gender discrimination and child abuse [1]; it is illegal in the United Kingdom and many other countries. It has profound and lifelong repercussions which include physical disfigurement, psychological trauma, pain, and reproductive and urinary tract complications.
Four types of female genital mutilation are described by WHO:
Type I – known as clitoridectomy, consists of partial or total removal of the clitoris:
Ia: removal of the clitoral hood or prepuce only
Ib: removal of the clitoris with the prepuce
Type II – known as excision, consists of partial or total removal of the clitoris and the labia minora, with or without labia majora:
IIa: removal of the labia minora only
IIb: partial or total removal of the clitoris and the labia minora
IIc: partial or total removal of the clitoris, the labia minora and the labia majora
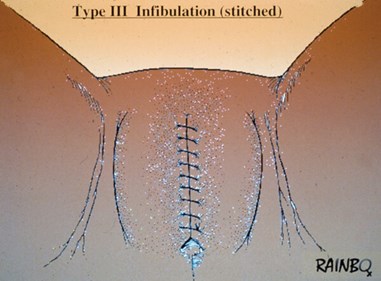
Type III – known as infibulation, consists of narrowing the vaginal opening by cutting and sewing the labia majora and / or the labia minora with or without clitoridectomy:
IIIa: removal and apposition of the labia minora
IIIb: removal and apposition of the labia majora
Type IV – Refers to any other harmful procedure to the female genitalia, non-required by medical purpose
The WHO estimates that the prevalence of women who have undergone female genital mutilation worldwide is more than 200 million and every year an estimated three million girls are at risk of undergoing the procedure. The majority of cases are concentrated in the western, eastern and north-eastern regions of Africa and also some countries in the Middle East and Asia [2].
The reasons for performing female genital mutilations vary from one region to another as well as over time. Commonly cited reasons are: a rite of passage to prepare a girl for adulthood and marriage, to ensure premarital virginity and marital fidelity, to reduce a woman’s libido in order to prevent extramarital relationships, cultural ideas of feminity and modesty, or a belief that the clitoris could cause a newborn’s death if its head is in contact with it [3]. In some places community leaders, religious leaders, and even medical personnel uphold such beliefs [4].
FGM is more often undertaken individually, but may occur in groups, and often accompanied by a ceremony which involves music, food and gifts where only women are allowed to be present. In the vast majority of instances there is no sterile environment, and analgesia and surgical instruments are not available. Instruments used include knives, clippers, scissors or hot objects. The same instrument is used on several women. The healing process is aided by application of ointments made from herbs, milk, ashes, sugar or animal excrement, which is thought to facilitate healing.
Despite global and regional attempts at ending this practice by making it unlawful and other interventions, the custom has persisted, and the multifaceted dynamic of its societal roots has made eradication of FGM difficult. Although the annual prevalence appears to be reducing, this practice continues to spread across the world with migrations of communities that practice FGM. Consequently, a substantial number of women affected by FGM live in countries such as the United Kingdom, France, USA and Canada. It is a public health concern that requires cultural competence to address, and in developed countries limited understanding of the cultural, religious and societal dynamics has made it difficult to deal with the practice [5,6].
Female genital mutilation leads to severe medical and psychological complications, and in some instances places the individual’s life at risk. Apart from the life-long health-related, ethical, moral and psychological consequences of FGM, it has been estimated by the World Health Organization that the obstetric and other health-related costs are significant [7].
In this review we outline some of the health-related ramifications of FGM and aim to focus on aspects that urologists may encounter.
Female genital mutilation: health consequences
From a health perspective, female genital mutilation is a major problem because of both immediate and long-term complications that arise from it and the need for surgical intervention; these have been well documented in the literature.
From a societal perspective, a history of female genital mutilation is commonly associated with high rates of co-occurring abuses such as domestic violence, forced marriage, child marriage, rape and torture [7].
Immediate complications include soft tissue infections with staphylococcus and other organisms, septic shock, tetanus (several documented cases), haemorrhage, severe pain, and death [3,5,8-11]. The method in which the FGM was carried out may determine the extent of the short-term complications. Limited access to healthcare in low income economies increases the mortality. Although data on mortality of girls who have undergone FGM is difficult to procure, it is thought that 1 in every 500 female circumcisions results in death.
Numerous delayed and long-term complications are known to occur. Psychological sequelae include sleep disorders, sexual dysfunction, depression, post-traumatic stress disorder (PTSD) and other psychological or psychiatric complications [12-14].
Long-term infectious complications include tetanus, human immunodeficiency virus (HIV), chlamydia trachomatis, herpes simplex virus and other sexually transmitted diseases [3,15]. Continued bacterial soft tissue infections can be responsible for septicaemia which can lead to death.
A common consequence is the formation of keloids and disfiguring scars such as synechiae or dermoid cysts which can be a source of anxiety and shame to the woman who has had FGM. Neuromas may develop from entrapped nerves within scar tissue which is a source of severe pain especially during intercourse. First sexual intercourse can only take place after gradual and painful dilation or cutting of the opening left after mutilation.
Gynaecological complications include cysts, haematocolpos and other menstrual problems, chronic pain, infertility, fistula and stenosis [3,12,15,16].
Sexual dysfunction is common, typically with dyspareunia, vaginismus, anorgasmia, and other symptoms [12,15-17].
Childbirth for infibulated women presents the greatest challenge and is associated with high maternal mortality rates and complications during labour with poor obstetric outcomes. These women are at higher risk of prolonged labour, severe perineal tears and fistulae. There is an increased incidence of episiotomy and caesarean section in these women [15,17]. A recent large retrospective study suggested that women who underwent infibulation may have a significant higher risk of eclampsia, but the mechanisms of such an association are unknown [18].
Urological aspects
Reports suggest urological complications are estimated to occur in at least a third of all female genital mutilation cases [19]. A three-year cross-sectional study from Egypt which was conducted from 2009 to 2012 compared a group of 251 women who underwent female genital mutilation to a 181 female control group and found a significantly higher prevalence of lower urinary tract symptoms (LUTS) in the FGM arm [21]. Reported LUTS include storage, voiding and post-micturition symptoms. Storage symptoms include, in order of frequency of occurrence: increased frequency of micturition, nocturia, urgency, mixed urinary incontinence, urgency urinary incontinence, stress urinary incontinence, voiding symptoms of intermittency, terminal dribbling, straining and slow stream, and post micturition symptoms such as a feeling of incomplete emptying and most-micturition dribbling. Symptoms depended on the type of FGM, with the highest odds ratio for FGM type III.
An anonymised survey of 30 women between the ages of 24 and 40 years living in the United States and who underwent female genital mutilation early in life reported significant impact on the quality of life from LUTS in 63% of the sample [22].
Urinary tract infections occur early and may persist [12,15,16,20]. As described above, the mutilation procedure often occurs in non-sterile environments using contaminated and reused instruments and is followed by application of various ointments and pastes. This frequently leads to infection immediately after. Subsequently, the disfigured anatomy may enable a change in the vaginal microbiota and long-term colonisation of the genitourinary system. Bladder outflow obstruction from urethral scarring hinders effective flushing out of organisms from the bladder. A study from Sudan reported commencement of recurrent urinary tract infections from a very young age; girls below seven-years-old with a history of FGM had a significantly higher risk of UTI with dysuria, spraying of the urinary stream and incomplete bladder emptying [21]. Lower urinary tract obstruction is most often caused by FGM type II and III [22].
Urinary stasis predisposes these girls to stone formation which may remain asymptomatic or have upper tract sequelae such as ureteric obstruction presenting with renal colic, and renal failure [23].
Urinary retention is mostly an immediate complication of female genital mutilation [24] and can either be a consequence of pain or bladder outlet obstruction from FGM type III. Urethral strictures may occur from damage to the urethra. The urethral meatus may be difficult to locate for catheterisation when this is indicated, consequent to either a very narrow introitus and / or meatal / urethral scarring.
Vesicovaginal fistula (VVF) after childbirth occurs from ischaemic necrosis of the vesicovaginal septum as a consequence of prolonged second stage of labour in women who have suffered FGM type III or any type of FGM – complicated by vulvar synechiae. The association between VVF and FGM remains debated in the absence of good quality evidence, and some studies have found no significant difference in the incidence of VVF in women with and without genital mutilation [25]. The occurrence of obstetric fistulae reflects the lack of access to safe and good quality obstetric care.
As this practice is illegal in many countries where FGM continues to occur, complications are underreported, especially in children. Victims of FGM are also likely to be taken to a healthcare facility for treatment. In some countries, health insurance may not cover such conditions, or the lack of affordability by the individuals concerned adds further barriers to treatment.
Management strategy
The range of urological complications caused by FGM requires specialist knowledge of FGM and its consequences, and a detailed appreciation of the anatomical aspects of reconstruction. The multifaceted psychological and physical issues demand a multidisciplinary approach to the management, with close collaboration between the urologist, gynaecologist, microbiologist, and therapists who specialise in the psychological and emotional aspects of PTSD. An independent interpreter may be required. A careful evaluation aiming to characterise the nature of the injuries enables counselling and treatment planning.
Even in an emergency situation a sensitive approach is essential because cultural influences are strong and FGM may be a taboo issue, in addition to the issues related to psychological and psychosexual effects of FGM. It is important to establish a relationship so that counselling and advice are effective.
Urinary tract infections are common in women following FGM and may be associated with bladder outflow obstruction from scarring of the introitus and urethra. Every effort should be made to establish a microbiological diagnosis, and investigations should be directed at identification and correction of bladder outlet obstruction. Investigations required may include a post-micturition scan, ultrasound for imaging of the renal tract, followed by targeted investigations such as cystourethroscopy, urethrograms or uroflowmetry.
FGM is commonly associated with long-term infections which include blood borne infections such as HIV and hepatitis B and C, vaginal infections, and chronic genital abscesses. Systematic evaluation with microbiology guidance is important.
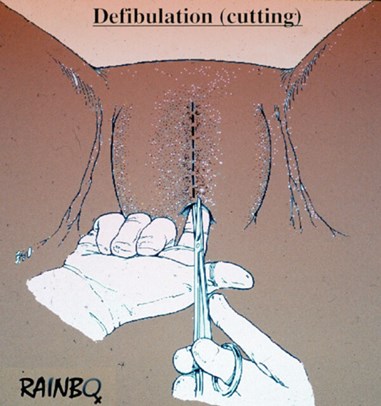
Management of urinary retention requiring catheterisation may pose difficulties in the presence of a sealed vulva, such as is frequently encountered in women who have had FGM type III / infibulation. These women may be found to have a small scarred vaginal opening or ‘pin-hole orifice’. In situations where the usual techniques prove impossible, an alternative technique known as the retraction technique has been described [26] which involves exposure of the urethral meatus with a Langenbeck retractor or a Sims speculum placed underneath the FGM scar and upward and outward traction to expose the external urethral meatus. Failing this, emergency defibulation may be required.
Defibulation refers to the surgical reopening of the vulva. This may be required for access to the urethra, or prior to childbirth if not already done prior to intercourse. Also known as Gabbar’s defibulation surgery, this may be performed under local anaesthesia and has been reported to improve urinary symptoms [27]. Defibulation should be scheduled soon after diagnosis to avoid emergency surgery. An alternative is the use of a CO2 laser which has been found to be particularly effective for the commonly encountered epidermal inclusion cyst [10]. There is however little or no data on the urological outcomes of defibulation [28]. Urethral strictures have been successfully managed by the use of clean intermittent self-catheterisation [29].
There is hardly any data on the outcomes of urethral reconstructive surgery after FGM [30]. In this case, defibulation is also the cornerstone of the management but other specific procedures may be considered (urethral dilatation or urethroplasty). Surgical management of FGM may involve clitoral reconstruction as described by Foldes [31]. This team from France reported reduction in pain and restoration of sexual function in a series of nearly 3000 women with limited results, depending on the extent (WHO type) of mutilation. Less than a third (29%) of the women returned for follow-up at one year. The authors report restoration of dignity and wellbeing of the women concerned. Surgery is however difficult in the presence of scarred or removed tissue and the reported outcomes of this case series have been challenged in a letter to the editor in the same issue of The Lancet.
Conclusion
Urologists need to be aware of the specific and complex issues related to female genital mutilation. This is a global health problem and is not uncommonly encountered in the United Kingdom. Women who have had FGM are more likely to be from economically deprived backgrounds and have complex social, religious and societal issues. Careful and sensitive evaluation should be followed by counselling and education on interventions that aim to prevent future complications. In some countries, healthcare systems and insurance providers do not recognise defibulation and clitoral reconstruction as therapeutic procedures and classify them as cosmetic surgery, which creates barriers to treatment. There remains a lack of data on the urological outcomes of FGM reversal surgery, and prospective studies are urgently required for this.
References
1. Momoh C. Female genital mutilation challenges for professionals. Eur Urol Today 2016:38.
2. World Health Organization. Classification des mutilations sexuelles féminines.
3. Oa A. Final Report on Position of Female Circumcision in Nigeria. News - Women’s International Network. 1981.
4. Ali C, Strøm A. “It is important to know that before, there was no lawalawa.” Working to stop female genital mutilation in Tanzania. Reprod Health Matters. 2012;20(40):69-75.
5. Vella M, Argo A, Costanzo A, et al. Female genital mutilations: genito-urinary complications and ethical-legal aspects. Urologia 2015;82(3):151-9.
6. Retzlaff C. Female genital mutilation: not just over there. J Int Assoc Physicians AIDS Care 1999;5(5):28-37.
7. Wikholm K, Mishori R, Ottenheimer D, et al. Female Genital Mutilation/Cutting as Grounds for Asylum Requests in the US: An Analysis of More than 100 Cases. J Immigr Minor Health 2020;22(4):675-81.
8. Knight R, Hotchin A, Bayly C, Grover S. Female genital mutilation--experience of The Royal Women’s Hospital, Melbourne. Aust N Z J Obstet Gynaecol 1999;39(1):50-4.
9. Barstow DG. Female genital mutilation: the penultimate gender abuse. Child Abuse Negl 1999;23(5):501-10.
10. Penna C, Fallani MG, Fambrini M, et al. Type III female genital mutilation: clinical implications and treatment by carbon dioxide laser surgery. Am J Obstet Gynecol 2002;187(6):1550-4.
11. Toubia N. Female Circumcision as a Public Health Issue. NEJM 1994;331(11):712-6.
12. Andro A, Cambois E, Lesclingand M. Long-term consequences of female genital mutilation in a European context: Self perceived health of FGM women compared to non-FGM women. Soc Sci Med 2014;106:177-84.
13. Behrendt A, Moritz S. Posttraumatic stress disorder and memory problems after female genital mutilation. Am J Psychiatry 2005;162(5):1000-2.
14. Utz-Billing I, Kentenich H. Female genital mutilation: an injury, physical and mental harm. J Psychosom Obstet Gynecol 2008;29(4):225-9.
15. Berg RC, Underland V, Odgaard-Jensen J, et al. Effects of female genital cutting on physical health outcomes: a systematic review and meta-analysis. BMJ Open 2014;4(11):e006316.
16. Berg RC, Underland V. Gynecological Consequences of Female Genital Mutilation/Cutting (FGM/C). Report from Norwegian Knowledge Centre for the Health Services (NOKC) No. 11-2014.
17. Lurie JM, Weidman A, Huynh S, et al. Painful gynecologic and obstetric complications of female genital mutilation/cutting: A systematic review and meta-analysis. PLoS Med 2020;17(3):e1003088.
18. Bellizzi S, Say L, Rashidian A, et al. Is female genital mutilation associated with eclampsia? Evidence from a nationally representative survey data. Reprod Health 2020;17(1):68.
19. Pycha A, Pycha A, Ladurner C, et al. Urological sequelae of female genital mutilation. Urol Ausg A 2018;57(10):1214-20.
20. Dehghankhalili M, Fallahi S, Mahmudi F, et al. Epidemiology, Regional Characteristics, Knowledge, and Attitude Toward Female Genital Mutilation/Cutting in Southern Iran. J Sex Med 2015;12(7):1577-83.
21. Almroth L, Bedri H, El Musharaf S, et al. Urogenital Complications among Girls with Genital Mutilation: A Hospital-Based Study in Khartoum. Afr J Reprod Health 2005;9(2):118-24.
22. Okwudili OA, Chukwudi OR. Urinary and Genital Tract Obstruction as a Complication of Female Genital Mutilation: Case Report and Literature Review. J Surg Tech Case Rep 2012;4(1):64-6.
23. Nour NM. Urinary Calculus Associated With Female Genital Cutting. Obstet Gynecol 2006;107(2):521-3.
24. Rouzi AA, Sahly N, Alhachim E, Abduljabbar H. Type I Female Genital Mutilation: A Cause of Completely Closed Vagina. J Sex Med 2014;11(9):2351-3.
25. Browning A, Allsworth JE, Wall LL. The relationship between female genital cutting and obstetric fistulae. Obstet Gynecol 2010;115(3):578-83.
26. Rouzi AA, Sahly N, Bahkali N, Abduljabbar H. Retraction technique for urinary catheterization of women with female genital mutilation. Eur J Obstet Gynecol Reprod Biol 2013;169(2):296-8.
27. Collinet P, Sabban F, Lucot J-P, et al. Prise en charge des mutilations génitales féminines de type III. J Gynécologie Obstétrique Biol Reprod 2004;33(8):720-4.
28. Effa E, Ojo O, Ihesie A, Meremikwu MM. Deinfibulation for treating urologic complications of type III female genital mutilation: A systematic review. Int J Gynecol Obstet 2017;136(S1):30-3.
29. Duncan D. Intermittent self-catheterisation for urolgical problems caused by FGM. Br J Nurs 2016;25(18):S26-S31.
30. Nour NM, Michels KB, Bryant AE. Defibulation to treat female genital cutting: effect on symptoms and sexual function. Obstet Gynecol 2006;108(1):55-60.
31. Foldes P. Reconstructive plastic surgery of the clitoris after sexual mutilation. Progres En Urol 2004;14(1):47-50.
TAKE HOME MESSAGE
- A sensitive and professional approach is required when dealing with urological complications of FGM. Healthcare practitioners should be sufficiently prepared.
- The earliest the diagnosis, the better the outcome.
- Proper microbial documentation should be seek for in cases of infection in order to avoid antibiotic resistance.
- Defibulation is the cornerstone of surgical management.
- Urologists should educate themselves on this topic and specific guidelines should be drawn up.
- Professionals should work in partnership and advocate against FGM.
Declaration of competing interests: None declared.








